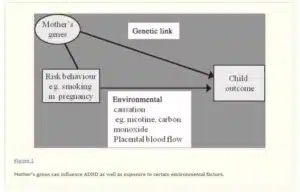
The study titled “Effects of hyperbaric oxygen at 1.25 atmospheres absolute with normal air on macrophage number and infiltration during rat skeletal muscle regeneration” explores the impact of hyperbaric oxygen therapy (HBOT) on the behavior of macrophages during the regeneration of rat skeletal muscle. Macrophages play a vital role in tissue repair and regeneration, and this research aims to investigate whether HBOT, which involves breathing oxygen under increased pressure, influences their activity and infiltration. This could provide insights into the potential therapeutic benefits of HBOT in the context of muscle healing.
Use of mild hyperbaric oxygen less than 2 atmospheres absolute (2 ATA / 2026.54 hPa) with normal air is emerging as a common complementary treatment for severe muscle injury. Although hyperbaric oxygen at over 2 ATA with 100% O2 promotes healing of skeletal muscle injury, it is not clear whether mild hyperbaric oxygen is equally effective. The purpose of the present study was to investigate the impact of hyperbaric oxygen at 1.25 ATA (1266.59 hPa) with normal air on muscle regeneration.
The tibialis anterior muscle of male Wistar rats was injured by injection of bupivacaine hydrochloride, and rats were randomly assigned to a hyperbaric oxygen experimental group or to a non-hyperbaric oxygen control group. Immediately after the injection, rats were exposed to hyperbaric oxygen, and the treatment was continued for 28 days. The cross-sectional area of centrally nucleated muscle fibers was significantly larger in rats exposed to hyperbaric oxygen than in controls 5 and 7 days after injury. The number of CD68- or CD68- and CD206-positive cells was significantly higher in rats exposed to hyperbaric oxygen than in controls 24 h after injury.
Additionally, tumor necrosis factor-α and interleukin-10 mRNA expression levels were significantly higher in rats exposed to hyperbaric oxygen than in controls 24 h after injury. The number of Pax7- and MyoD- or MyoD- and myogenin-positive nuclei per mm2 and the expression levels of these proteins were significantly higher in rats exposed to hyperbaric oxygen than in controls 5 days after injury. These results suggest that mild hyperbaric oxygen promotes skeletal muscle regeneration in the early phase after injury, possibly due to reduced hypoxic conditions leading to accelerated macrophage infiltration and phenotype transition. In conclusion, you got the asnwer of Effects of hyperbaric oxygen at 1.25 atmospheres mild hyperbaric oxygen less than 2 ATA with normal air is an appropriate support therapy for severe muscle injuries.
FAQs
Q1: What is hyperbaric oxygen therapy (HBOT), and how does it work?
A1: HBOT is a medical treatment that involves breathing pure oxygen in a pressurized chamber. This increased pressure allows the body to absorb more oxygen, promoting various therapeutic effects, including enhanced tissue repair.
Q2: Why are macrophages important in the context of skeletal muscle regeneration?
A2: Macrophages are immune cells that play a critical role in the inflammation and repair processes during tissue regeneration. They help remove damaged tissue and promote the growth of new muscle fibers.
Q3: What were the findings of the study regarding the effects of HBOT on macrophage behavior in skeletal muscle regeneration?
A3: The study investigates the impact of HBOT at 1.25 atmospheres absolute with normal air on macrophage numbers and infiltration during muscle regeneration in rats. The findings may reveal whether HBOT influences macrophage activity and contributes to muscle repair.
Q4: What are the potential implications of this research for muscle regeneration and HBOT as a therapeutic approach?
A4: If the study shows that HBOT influences macrophage behavior positively in muscle regeneration, it may suggest a potential therapeutic application of HBOT to enhance muscle healing and recovery in various clinical contexts.
Conclusion
The research on the effects of hyperbaric oxygen therapy at 1.25 ATA with normal air on macrophage behavior during rat skeletal muscle regeneration holds promise for understanding the potential benefits of HBOT in tissue repair. The role of macrophages in the healing process is pivotal, and if HBOT can positively influence their behavior, it may open new avenues for improving muscle recovery in various medical scenarios. Further studies and clinical research are needed to fully explore the therapeutic applications of HBOT in this context.