This article presents a genome-wide microarray analysis of gene expression in human microvascular endothelial cells (HMEC-1) exposed to Hyperbaric oxygen induces a cytoprotective, designed to simulate clinical conditions. The study identified significant changes in gene expression, with a focus on immediate early transcription factors, metallothioneins, and molecular chaperones. Pathway analysis revealed the Nrf-2-mediated oxidative stress response as a primary responder to HBOT. The study confirmed these changes using quantitative PCR and found that HBOT increased cell proliferation, oxidative stress resistance, and endothelial tube formation. This research sheds light on the mechanisms of HBOT’s effects on endothelial cells and suggests potential applications for improving wound-healing protocols and patient preconditioning before surgery.
A genome-wide microarray analysis of gene expression was carried out on human microvascular endothelial cells (HMEC-1) exposed to hyperbaric oxygen treatment (HBOT) under conditions that approximated clinical settings. Highly up-regulated genes included immediate early transcription factors (FOS, FOSB, and JUNB) and metallothioneins. Six molecular chaperones were also up-regulated immediately following HBOT, and all of these have been implicated in protein damage control. Pathway analysis programs identified the Nrf-2-mediated oxidative stress response as one of the primary responders to HBOT. Several of the microarray changes in the Nrf2 pathway and a molecular chaperone were validated using quantitative PCR.
For all of the genes tested (Nrf2, HMOX1, HSPA1A, M1A, ACTC1, and FOS), HBOT elicited large responses, whereas changes were minimal following treatment with 100% O2 in the absence of elevated pressure. The increased expression of immediate early and cytoprotective genes corresponded with an HBOT-induced increase in cell proliferation and oxidative stress resistance. In addition, HBOT treatment enhanced endothelial tube formation on Matrigel plates, with particularly dramatic effects observed following two daily HBO treatments. Understanding how HBOT influences gene expression changes in endothelial cells may be beneficial for improving current HBOT-based wound-healing protocols. These data also point to other potential HBOT applications where stimulating protection and repair of the endothelium would be beneficial, such as patient preconditioning prior to major surgery.
FAQs for Hyperbaric oxygen induces a cytoprotective
Q1: What is hyperbaric oxygen therapy, and how does it induce a cytoprotective and angiogenic response in human microvascular endothelial cells?
A1: Hyperbaric oxygen therapy (HBOT) is a medical treatment that involves breathing pure oxygen at increased atmospheric pressure. When applied to human microvascular endothelial cells, HBOT can stimulate a cytoprotective response, which means it enhances the cells’ ability to resist damage and stress. Additionally, it induces an angiogenic response, promoting the formation of new blood vessels, which is essential for tissue repair and healing.
Q2: Why is it important to understand the cytoprotective and angiogenic effects of hyperbaric oxygen on human microvascular endothelial cells?
A2: Understanding these effects is crucial because they have significant implications for various medical applications. Enhancing the cytoprotective response can improve cell survival and resistance to injuries, while promoting angiogenesis is vital for wound healing and tissue repair. This knowledge can lead to more effective treatments and therapies.
Q3: What are the potential clinical applications of hyperbaric oxygen therapy in light of its cytoprotective and angiogenic effects on human microvascular endothelial cells?
A3: HBOT is already used in various clinical applications, including the treatment of conditions such as diabetic ulcers, carbon monoxide poisoning, and chronic wounds. The understanding of its cytoprotective and angiogenic effects may further expand its use in wound healing and preconditioning before surgery, among other potential applications.
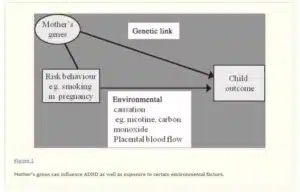
Q4: Are there specific genes or pathways involved in the cytoprotective and angiogenic responses induced by hyperbaric oxygen in these cells?
A4: Yes, studies have identified specific genes and pathways that play a role in these responses. For example, the Nrf-2-mediated oxidative stress response is one of the primary pathways activated by HBOT. Various immediate early genes and molecular chaperones are also upregulated in response to hyperbaric oxygen, contributing to the cytoprotective effect.
Q5: Is hyperbaric oxygen therapy considered a safe and effective treatment for these cellular responses?
A5: HBOT is generally considered safe when administered by trained medical professionals. Its effectiveness depends on the specific medical condition being treated and the individual patient’s response. It has been shown to be effective in various applications, but its suitability for a particular patient should be determined by a healthcare provider.
Conclusion
The study underscores the remarkable potential of Hyperbaric oxygen induces a cytoprotective and angiogenic response in human microvascular endothelial cells. These findings shed light on the therapeutic possibilities of hyperbaric oxygen therapy, not only in enhancing cellular resilience but also in fostering the formation of new blood vessels, a crucial process in tissue repair and regeneration. This research provides valuable insights into the mechanisms underlying hyperbaric oxygen’s benefits, with implications for a wide range of medical conditions where promoting angiogenesis and cytoprotection could play a pivotal role in improving patient outcomes and overall health. Further exploration of these mechanisms holds promise for future medical advancements.